Dr. Sandoval came back on Saturday (I think it was Saturday). I asked him what in the world he was thinking, going on vacation when we weren't actually out of the hospital yet, and he promised he won't do it again. Faith re-started feeds Friday, at 6 mL every 3 hours, then stopped on Saturday morning because she threw up. She had still been pooping out a lot of barium, and it was very thick and pasty, like caulk. I think it was plugging her up, and so it was easier for stuff to come back up than go through.
I was going to suggest at that point that we should re-start the enemas, to help clear some of that out, but was waiting to see a doctor. Dr. Hall came in then, and asked what I thought was going on, and I told him my theory about her being stopped up, and he said we should go ahead and get an x-ray and probably re-start the enemas. The x-ray wasn't promising, it showed that she still had barium in her stomach, 3 days after the UGI. I find it very interesting and reassuring that Dr. Hall and I think along the same lines, that we think the same things before either one of us brings anything up.
Saturday afternoon feeds were re-started, and she worked up to getting 24 mL every 3 hours last night around midnight, before she started throwing up and just not tolerating them. She screamed every time we fed her yesterday, and has just really seemed like her reflux is bugging her more.
So, since she threw up quite a bit last night, they stopped feeds again, and then re-started them this morning, just doing trophic feeds of 6 mL every 3 hours, just to keep her happy and not feeling super hungry and fussy.
They also started some Maalox for her reflux, so now she's on that, IV Protonix, and Reglan for reflux (and Colic Calm- a homeopathic medicine we are trying). Other than that, she's on Ursodiol for her cholestasis, Nystatin to keep her from getting an infection w/ her Broviac, and they started her on Gentamicin today, an antibiotic to help with bacterial overgrowth in her intestines, since that is common in people with intestinal dysmotility. They'll alternate the Gentamicin with another antibiotic every other week to treat that, and when she gets her Broviac removed, we'll get her on probiotics to help increase the number of good bacteria in relation to the bad bacteria, and get her gut a little healthier.
So, Monday's meeting went pretty well, and we do have our plan now. We decided on Monday that since Faith did so well the last time we worked her up on feeds, we'd give her a chance to potentially do well again and see if it would work, but that we didn't want to wait too long or waste time, when we know what her problem is, and they think they can fix it.
Her problem is essentially that she has a section of intestine, about a 12-18 inches long, that is very dilated, and then the stuff downstream from that is still smaller than normal. The dilated section is the part right out of the stomach, so it is a part that is very important for nutritional absorption. If that section was shorter, they would consider just taking it out, but since it is longer, it wouldn't be good for her to lose that much intestine. This is a re-creation of the picture Dr. Partrick drew to show us what her intestine looks like:
 So, what they're going to do, since they can't just take the dilated part out, is a surgery called Tapering Enteroplasty. The next picture is my attempt at showing what they'll be doing. The black dotted line is where they'll staple the intestine, using titanium staples that will stay in forever, to make the diameter smaller. They'll put a catheter in first, to be sure they get it to the diameter they want. Then the part with the blue lines through it will come off. They'll also remove the section between the red dotted lines, where the dilated section meets up with the smaller section, because they think there may be the beginning of an atresia there that didn't fully develop into an atresia. So just to be safe, they're going to take that part out.
So, what they're going to do, since they can't just take the dilated part out, is a surgery called Tapering Enteroplasty. The next picture is my attempt at showing what they'll be doing. The black dotted line is where they'll staple the intestine, using titanium staples that will stay in forever, to make the diameter smaller. They'll put a catheter in first, to be sure they get it to the diameter they want. Then the part with the blue lines through it will come off. They'll also remove the section between the red dotted lines, where the dilated section meets up with the smaller section, because they think there may be the beginning of an atresia there that didn't fully develop into an atresia. So just to be safe, they're going to take that part out.
At the care conference, they weren't for sure going to do the surgery, but were going to go ahead and schedule it so that they could do it if they needed to. After last night, surgery is for sure, and will be on Tuesday afternoon. We would love it if they could do it sooner, but Dr. Partrick is out of town until then, so that is the soonest it can be. Faith also has low hematocrit, so she'll need another blood transfusion before the surgery, and my dad isn't coming until Friday to donate blood for her, so it actually works out pretty well to have the surgery on Tuesday, since the blood will be ready on Monday.
The goal of the surgery is to make her small intestine a more consistent size, because the dilated part isn't able to work the way it should. Once it is a more normal size, the muscles should be able to work better to move food through. The barium in her stomach still after the UGI would make you think that she has a stomach emptying problem, but Dr. Partrick thinks it is probably more to do with the fact that the dilated part of intestine is right after the stomach, and stuff just moves through there so sluggishly that the stomach can't empty as quickly as it should, since there's nowhere for the stomach contents to really go.
Hopefully, she should be able to start feeds again about 5-7 days out from surgery, and hopefully this time things will go a little better and she'll be able to work up to the big amounts and have everything working the way it should. Best case, she'll be able to work up to full feeds, taken 100% by mouth. If she isn't, our next option is to work her up to the biggest amount she can take orally, and make the rest up with TPN, provided her liver numbers continue to get better once her TPN amount is decreased. The last option, the one we want to avoid if at all possible, would be that if she can't take 100% feeds by mouth, and her liver continues to have problems from the TPN, they would put in a feeding tube and make the rest of her nutrition up with continuous feeds at night. If we had to go this route, we would probably insist on an NG tube, in hopes that we could get her up to bigger amounts without needing to get a g-tube.
We're optimistic that things will go best case scenario, and if they don't, we're hoping her liver stays fine so we can do the second option. (And, this week her direct bilirubin did go down, from 11.8 to 5.6, and her other liver function numbers got better too, which is wonderful news.) They will also be doing a liver biopsy during the surgery on Tuesday, to give a better picture of how her liver really is. I know a lot of people, especially people who already have g-tubes, would question our decision regarding preferring TPN over a g-tube... but I guess we are just afraid that doing a tube would potentially interfere with or eliminate Faith's desire to eat. Eating is the one thing that Faith has truly excelled at, to everyone's surprise and excitement, so we want to do everything we possibly can to protect that.
Please keep us in your thoughts and prayers this week as we approach the most important (and hopefully LAST!) surgery yet...








1 comment:
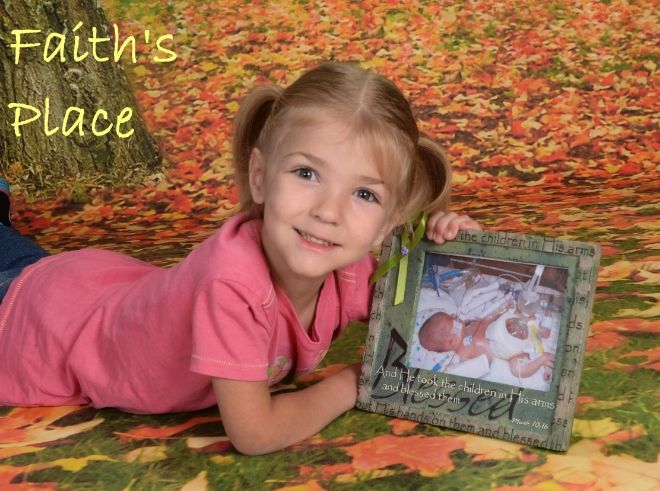
I'm glad everyone is on the same page and you have a plan. It is amazing how big Faith is getting (at least it looks like it in the pictures). I am hoping this will be Faiths last surgery and she can begin to nurse quickly. Your strength is admirable. Your in my thoughts.
Post a Comment