This post is a reflection, a way for me to remember and process the events that happened on September 11, 2008, and how our lives have changed since then. If you don't read all the way through, please at least scroll to the end of the post, to see how you can help others during their gastroschisis journeys. It will only take a minute, and it's free! Thank you to everyone who has read the blog, commented, and supported us through these past couple of years!!!
September 11, 2008:
On September 10, I had an ultrasound and a midwife's appointment. I was 28 weeks pregnant, planning a homebirth, and everything in my pregnancy was going perfectly. But I had a fear I couldn't shake that there might be something wrong with the baby, which was what prompted the ultrasound. The ultrasound was first, and it was sort of strange... they had told us to be ready for it to take about an hour. It took 20 minutes. The tech moved around a lot, and never kept it in one place for too long. We got 4 pictures of our baby's head, and no full body profiles. And afterwards, they had us wait while the radiologist looked at the preliminary report to decide if they needed to do anything else. I brushed it all off as nothing... (I was still having morning sickness at that point and wasn't feeling well, and was mostly just disappointed that it had gone so quickly, and we didn't get a DVD of it like I had with Noah.)
I went to my appointment with the midwife. She said they had called about the ultrasound, wanting to talk to the other midwife and trying to figure out how to get them the report or something, but it was weird... she said to try not to be worried about it, and it was probably just because they weren't used to working with homebirth midwives. My appointment was fine, everything continued to be perfectly normal.
The more I thought about the ultrasound and how strange it was, the more I worried. I called the midwives a few times to see if they had gotten the report yet. They said no, but if it was something to worry about, they were sure they would have heard it already...
September 11, I had an appointment with my family doctor. She had done some bloodwork to try and figure out what was causing my constant pain and fatigue. The bloodwork was fairly straightforward, except that my CRP (a measure of inflammation) was elevated, and my ANA (an autoimmune marker) was positive, with a pattern that suggested I may have Lupus. I asked if that would risk me out of a homebirth... she said she didn't think so, but that it would depend on what a rheumatologist thought. I am very blessed to have a family doctor who supports homebirth

At the end of the appointment, we mentioned how strange the ultrasound had been, and that we still hadn't heard anything. The doctor called over to get the report, while we went out to the waiting room. (Dave was at work, my mom was with me.)
A few minutes later, the nurse came and got my mom and I, and sat in the waiting room with the boys... It confirmed what I had suspected, I knew something was wrong. My doctor told us the baby had gastroschisis. She said that I would have to transfer care to a high-risk OB practice, and that the baby would have to be at Children's Hospital in Denver, because there are no pediatric surgeons in Northern Colorado. She said I would probably have to have a c-section scheduled around 36 weeks... I think she was nearly as heartbroken as I was to have things go completely in the opposite direction of how I wanted them to go.
I was a mess. My mom took me to see Dave at his office, so I could tell him in person... We stood in the parking lot, hugging and crying. I knew at that moment that if the baby was a girl, her name would be Faith (which I had thought all through my pregnancy, but Dave had fought me on).
I couldn't sleep or eat after that. I called the midwife to tell her the news. She was amazing, and offered to support us as a doula (an offer I wish I would have accepted, in hindsight!). I was so crushed at the moment, and so sure that my only option would be a scheduled c-section, that I turned her down. I stopped reading the birth books I had been reading, and told Dave he didn't have to read anymore, either, because I was sure that we wouldn't get to have any semblance of a birth I would be happy with, anyway, and I didn't want to continue preparing myself if I was only going to be disappointed in the end.
I searched and found a program through University and Children's Hospitals in Aurora that connects high-risk moms with all of the providers they will need, before and after birth, and I scheduled an appointment with the perinatologists at University. I was shocked when they said they wouldn't be able to get me in for nearly an entire month! I spent the next month in worry, not knowing what was going on, constantly afraid that my baby was going to die, or that I was going to go into preterm labor and we would be separated.
The downside of educating yourself is that you learn all of the bad things that could happen... and gastroschisis and lupus both have their own sets of very real risks for babies. There is a 10% risk of stillbirth with gastroschisis, and a source I found cited a 25% risk of stillbirth or premature labor with lupus. I figured if you added them together, my baby probably only had about 65% chance to make it to full term and live... probably not good math, but it's how my pregnant, worried brain worked.
Finally the perinatologists saw me at 32 weeks. They made me feel completely stupid for having planned a homebirth, and acted like I really had nothing to worry about. The good thing was, they did a much more detailed ultrasound, and it showed that other than the gastroschisis, there was nothing wrong with our baby. And it confirmed that the baby was a girl. (We originally didn't want to know, so we hadn't found out at the first ultrasound. But we decided gastroschisis was enough of a surprise, and with how sure I was in my mind that the baby was going to die, I wanted to have a name picked out.) They also assured me I could have a vaginal birth!
I continued having weekly appointments, weekly ultrasounds to check bloodflow through the placenta and cord, weekly checks of the amniotic fluid level, twice weekly NST's, and bi-weekly ultrasounds to check growth... During this time, my mom and I lived with Nathan and Noah in my parents' camper, in a campground near the hospitals. I had decided that I wanted to be there, so that if I went into preterm labor, I would be able to be at the hospital right next door to Faith, so that I would be able to be with her as soon as possible after she was born. I didn't want us to be separated more than I knew we already would be.
I was completely cut off from my normal life, from my friends, and from everything I had wanted. I'm sure I was depressed, but I was also so tired and in so much pain from the "lupus" that I attributed most of it to that. I saw a rheumatologist who said she thought it probably was lupus, but that she didn't think it was smart to start me on medication until after the baby was born, since I was 32 weeks pregnant and most gastroschisis babies are born around 36 weeks... 4 more weeks wouldn't hurt anything, and it would probably be better for Faith not to expose her to anything additional.
36 weeks came, and I fully expected the perinatologists to schedule me for an induction. They didn't. They wouldn't, even when I asked them to (because the research I had read related bowel damage to prolonged exposure to the amniotic fluid, especially in the presence of meconium, which the risk for greatly increases the longer you are pregnant). They did an amniocentisis at 37 weeks to check for lung maturity. It was very painful, in such a weird way... It felt like someone punched me in the uterus- like *directly* in the uterus. Like they took it out and punched it. They also poked Faith in the process of collecting the fluid (she actually had a mark on her back from it for over a month after she was born!). I hurt for the whole rest of the day, while I waited for the results that I was hoping (for the baby's sake) would mean an induction the next day. They called to say it was "negative". No number result, nothing beyond the word negative. Oh, and they said they had a hard time testing it, because there was meconium in the fluid. The very reason I was wanting to be induced. (I wonder now if they thought I was just sick of being pregnant... but honestly, would a mom who had been planning a homebirth *really* be begging for an induction? Any educated mom knows an induction greatly reduces your chances of having a vaginal birth, in addition to being incredibly more painful than a natural labor...) And of course, this was on a Friday afternoon.
I spent the weekend worried about the baby, looking up research study after research study that supported my wishes to be induced (especially in the presence of meconium) and writing down the citations to take to the doctor, to try and talk them into it. I actually ended up going to L & D for something (I can't remember what), where they explained that it WASN'T meconium in the fluid, it was actually just bile, which you would expect when the intestines are freely floating in the fluid. I was scheduled for an induction the following Friday, at 38 weeks. I was planning a drug-free induction, using a foley bulb and nipple stimulation, if needed... thankfully it didn't come to that. (Apparently, if you threaten me with induction, I go into labor...)
On Wednesday I went in for my 38 week appointment. I told the OB I had lost my mucus plug, and that I thought I was in early labor. She checked me, and said my cervix was exactly the same as it had been (which wasn't much of anything in terms of dilation or effacement), and that I probably wasn't in labor, and they'd see me on Friday for the induction. Wednesday night around 10, I told my mom she'd better get some sleep, because I knew I was in labor. I managed to sleep until about 2 am... I woke up to go to the bathroom and was having regular painful contractions. I waited about a half hour before waking my mom up. If we had been somewhere more conducive to laboring, and less likely to wake up two 2 year old boys with my moans, I'm sure I would have waited much longer to go to the hospital... especially since we were so close. As it was, Dave and my dad had an hour drive to get to us, so it was about 4 by the time Dave, my mom, and I got to the hospital.
The labor was so intense. I was sure I was going to be at 6-7 cm, because it felt like I was in transition. I recognize now that the intensity of my labor probably had a LOT to do with all of the fears I had surrounding this birth and what would happen to Faith afterwards. One of the many reasons I should have taken Kim up on her offer to be our doula... I was only 4 cm, but contracting regularly, so they admitted me. I had to be on the monitor continuously. I didn't even know telemetry monitors existed, and never asked about it, so I was essentially "chained" to the machine, and had about a 2-3 foot radius for mobility. Of course, because I was on the monitor, that meant I couldn't use the tub or shower for relief...
I had SO much hip pain. I never really focused on how Faith was positioned while I was pregnant... it's funny, I could draw you a picture on my belly to show you exactly how Noah was positioned, but I honestly have no idea of where Faith was. I knew she was head down, and that is pretty much all that mattered at the time... and because I knew her intestines were floating around in there, I was very hesitant to feel around like I had with Noah to figure things out... thinking of how much pain I was in, and knowing after the fact that she had been tangled up in her cord, which kept her from descending, I'm sure she was positioned pretty funky. Also, my cervix was dilating even though it wasn't effacing, which may have had something to do with it as well...
Sometimes I'm still amazed by how present God was in the whole situation. Probably at least 6 or 8 times during labor, they checked me to see if they could break my water and help things progress. Faith was still floating each time, so they couldn't. The one time they thought they could, the doctor actually had the hook in hand before deciding at the last second not to... I think that decision not to do it saved us from a cord prolapse and emergency c-section, since we knew after Faith was born that she'd had the cord all wrapped around her head (she had bruising across her face from it, and it was around her neck at birth).
Since I wasn't making any real progress, and they weren't able to break my water to see if it might help, they started mentioning the possibility of a c-section. I decided that if they were going to end up doing a cesarean anyway, I might as well get the epidural and see if it might help... Because I was high-risk, the anesthesiologist had been required to come up and introduce himself, and explain the epidural to me when I was admitted. At the time, I had blown him off, assuring him I wouldn't need his services because we were planning a natural birth... so when he came back to give me the epidural, I think he felt sorry for me. He gave me a VERY light one, so I could still feel every contraction, only they were painless. I could still move and feel my legs, all the way down to my toes. I just didn't have the awful pain anymore.
The epidural allowed me to relax. I was so exhausted, and the pain had been so bad... the relief from it was enough to make me stop thinking about everything that was going to happen after Faith was born, and suddenly my body started making progress. My water broke on its own about 20 minutes after the epi was in. Probably 15 minutes after that, I started pushing the "boost" button on it, as I was feeling TONS of pressure. They came in and checked me, and I was complete and ready to push. I loved that I could feel everything- I totally had the urge to push, and I felt Faith sliding down and out...
I only pushed a few times before Faith's head was born, with the cord wrapped tightly around her neck. (Interestingly enough, despite all of her cord antics AND the epidural, her heart rate stayed perfectly stable throughout the entire labor.) As the doctor went to unwrap the cord, the rest of her was born, and the cord broke right where it attached on her belly. Immediately she was whisked away to be assessed by the 20 or so neonatologists and neonatal nurses and nurse practitioners, while they simultaneously worked to stop the bleeding from her severed umbilical blood vessels (there was NOTHING there to clamp!). All my mom, Dave and I noticed was how HUGE and purple her intestines were... none of us could imagine how they would be able to get them into her tiny body.
A little while later, they brought her over to show her to me, before they took her away to the NICU... I was able to touch her head and give her a kiss before she left the room. Within 2 hours, she was baptized and on her way to Children's for her first surgery. Less than 12 hours after her birth, I was discharged and next door at Children's with her. The road since then has been a very winding one, with lots of ups and downs. None of us could have predicted how things would go, or where we would end up...
The most amazing thing to me is that it has already been 2 years since all of this started... It seems like it was just yesterday. A lot of parents who have been through similar struggles with their children say that once you are on the other side, it will all be a distant memory... I'm wondering when that is supposed to happen. It is all so fresh. The feelings are right there, and as we go into September 11, I can remember exactly how I was feeling 2 years ago...
We were lucky to have the support of family and friends through everything we experienced. But I didn't have anyone really who had been through what we were going through. There were a couple of blogs that I found and read, but that was about it. Thankfully, families going through this journey now have a wonderful organization called Avery's Angels to support them. I am proud to be a part of this organization, to offer new parents support and advice as they travel their own twisting, turning roads through a gastroschisis pregnancy and NICU stay... If you would like to do something to help these families, please consider voting for Avery's Angels in the Pepsi Refresh campaign, spreading our story, and asking your friends to vote, too. Go to www.refresheverything.com/averysangels4gastroschisisbabies EVERY DAY and vote, or text 101825 to 73774...
And as you remember your own experiences from September 11, think of ours, and how in an instant, our lives turned upside down. Be thankful for what you have, hug your kids, and remember to live in the moment... while also knowing that if something unexpected does happen, you will get through to the other side, and hopefully you will be a stronger, better person from the journey.
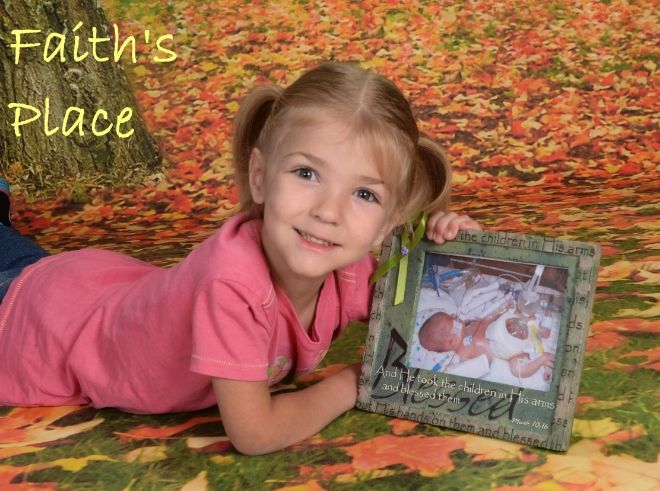
Faith at birth:
Faith today, September 10, 2010: